Get our email updates
Stay up-to-date on the companies, people and issues that impact businesses in Syracuse, Central New York and beyond.
What's New
Upcoming Events
CNYBJ Job Board

NIH awards Bassett Research Institute multimillion dollar grant
COOPERSTOWN, N.Y. — The National Institutes of Health (NIH) has awarded the Bassett Research Institute’s Center for Rural Community Health a multi-year grant to study

NOCO continues installing energy efficient lighting at 45 Tops stores
SYRACUSE, N.Y. — The Energy Solutions team at NOCO is working to install energy-efficient lighting at 45 stores of Tops Friendly Markets throughout New York state. NOCO is an energy company based in Tonawanda that has a local office at 1300 Wolf St. in Syracuse. The installation project, which started back in February and is
Get Instant Access to This Article
Become a Central New York Business Journal subscriber and get immediate access to all of our subscriber-only content and much more.
- Critical Central New York business news and analysis updated daily.
- Immediate access to all subscriber-only content on our website.
- Get a year’s worth of the Print Edition of The Central New York Business Journal.
- Special Feature Publications such as the Book of Lists and Revitalize Greater Binghamton, Mohawk Valley, and Syracuse Magazines
Click here to purchase a paywall bypass link for this article.
SYRACUSE, N.Y. — The Energy Solutions team at NOCO is working to install energy-efficient lighting at 45 stores of Tops Friendly Markets throughout New York state.
NOCO is an energy company based in Tonawanda that has a local office at 1300 Wolf St. in Syracuse.
The installation project, which started back in February and is now more than halfway complete, includes converting all interior and exterior lighting to LED (light-emitting diode.), per the company’s Sept. 30 announcement.
Once these lighting upgrades are completed later this year, NOCO and Tops estimate annual savings of more than 16 million kilowatt hours or about $1.6 million on electricity costs.
“At Tops, we are deeply committed to sustainability and responsible energy use, and this partnership with NOCO is another step forward in reducing our environmental footprint while enhancing our in-store experience,” Ron Ferri, president of Tops Markets, said in the NOCO announcement. “The transition to energy-efficient LED lighting not only supports our long-term operational goals but also helps us create a brighter, more welcoming environment for our customers and associates. We’re proud to lead with initiatives that deliver real impact for our communities and the planet.”
The project in the impacted stores involves new lighting in customer-facing, backroom, and loading dock areas, including coolers, freezers, and deli cases.
With this current project, Tops is responsible for paying about 36 percent of the total $4.7 million project cost, offsetting the remaining balance with available energy incentives and rebates through utility-efficiency programs in the geographic areas where the stores are located.
“If you run a business, there are always factors outside of your control and rising electric prices are one of them, with no end in sight to continued rate increases,” Michael Casciano, president and COO of NOCO, said. “NOCO is committed to helping businesses optimize their energy usage while also reducing their energy costs. While Tops is already starting to see the cost benefits of their lighting conversion, these upgrades have also enhanced the quality of light within the stores, creating a more comfortable and appealing environment for their customers and employees.”
Since 2019, Tops has been working to retrofit stores to LED lighting in addition to converting its parking lot lights and fuel station canopies across the chain’s footprint to LED fixtures to reduce energy consumption. When the lighting conversion is completed at these 45 Tops stores, about 121 of the grocer’s stores will have been upgraded.
In recent years, Tops has reduced its electric consumption by 11.5 percent with various energy-saving initiatives involving mostly LED lighting, NOCO said.
NYS home sales flat in September but pending sales jump
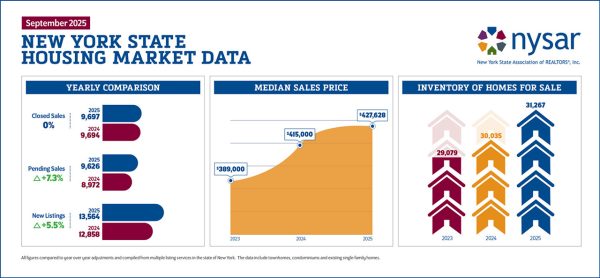
ALBANY, N.Y. — Realtors in New York state closed on the sale of 9,697 previously owned homes in September, virtually unchanged from the 9,694 homes they sold in the year-earlier month. However, pending sales increased more than 7 percent in the ninth month of 2025, possibly foreshadowing a rise in closed sales in the next
Get Instant Access to This Article
Become a Central New York Business Journal subscriber and get immediate access to all of our subscriber-only content and much more.
- Critical Central New York business news and analysis updated daily.
- Immediate access to all subscriber-only content on our website.
- Get a year’s worth of the Print Edition of The Central New York Business Journal.
- Special Feature Publications such as the Book of Lists and Revitalize Greater Binghamton, Mohawk Valley, and Syracuse Magazines
Click here to purchase a paywall bypass link for this article.
ALBANY, N.Y. — Realtors in New York state closed on the sale of 9,697 previously owned homes in September, virtually unchanged from the 9,694 homes they sold in the year-earlier month.
However, pending sales increased more than 7 percent in the ninth month of 2025, possibly foreshadowing a rise in closed sales in the next couple of months. That’s according to the New York State Association of Realtors’ (NYSAR) September housing report issued on Oct. 23.
“Key indicators such as new listings and pending sales increased in September while housing inventory across New York escalated for the seventh consecutive month,” NYSAR said to open the housing report.
Mortgage rates showed signs of moving lower heading into the fall. NYSAR cited Freddie Mac as indicating the average 30-year fixed rate at 6.35 percent in September 2025, down from 6.59 percent in August 2025. A year earlier, in September 2024, the average 30-year rate stood at 6.18 percent. Freddie Mac is the more common way of referring to the Virginia–based Federal Home Loan Mortgage Corporation.
New York sales data
Statewide housing inventory reached 31,267 units in September, a 4.1 percent increase from September 2024’s total of 30,035 available homes. This marks seven straight months of increasing housing inventory statewide, NYSAR noted.
New listings of existing homes available for sale in the Empire State rose 5.5 percent to 13,564 this September from 12,858 in September 2024.
The months’ supply of homes for sale at the end of September stood at 3.5 months’ supply, up 3 percent from 3.4 months a year prior, per NYSAR’s housing report.
A 6 month to 6.5-month supply is considered a balanced market, the association stipulates.
Pending sales totaled 9,626 in September, a jump of 7.3 percent compared to the 8,972 pending sales in the same month in 2024, according to the NYSAR data.
Home sales prices across the Empire State continue to climb in the latest month. The median home sales price was $427,628 in September, up 3 percent from the $415,000 median price tag in September 2024.
All home-sales data is compiled from multiple-listing services in New York, and it includes townhomes and condominiums in addition to existing single-family homes, according to NYSAR.

DRI to help downtown Norwich get a new boutique hotel
NORWICH, N.Y. — The upcoming Principle Hotel, an $8.3 million boutique hotel in downtown Norwich, is among the projects that the community is developing as part of its funding award in the state’s Downtown Revitalization Initiative (DRI). Officials in Norwich held an Oct. 23 groundbreaking for the hotel. The Principle Hotel will have 61 rooms
Get Instant Access to This Article
Become a Central New York Business Journal subscriber and get immediate access to all of our subscriber-only content and much more.
- Critical Central New York business news and analysis updated daily.
- Immediate access to all subscriber-only content on our website.
- Get a year’s worth of the Print Edition of The Central New York Business Journal.
- Special Feature Publications such as the Book of Lists and Revitalize Greater Binghamton, Mohawk Valley, and Syracuse Magazines
Click here to purchase a paywall bypass link for this article.
NORWICH, N.Y. — The upcoming Principle Hotel, an $8.3 million boutique hotel in downtown Norwich, is among the projects that the community is developing as part of its funding award in the state’s Downtown Revitalization Initiative (DRI).
Officials in Norwich held an Oct. 23 groundbreaking for the hotel.
The Principle Hotel will have 61 rooms and include a rooftop lounge, restaurant, and event room, “so visitors can stay and enjoy the unique retail, dining and entertainment options in downtown Norwich,” the New York State Department of State said in an announcement.
The 12,000-square-foot property at 14-16 South Broad St., was once part of the SUNY Morrisville campus. It will soon become a boutique hotel that will include a dining area, lounge, conference room, fitness center, outdoor patio, and open courtyard with a fountain.
“This hotel represents far more than a new place to stay — it’s a cornerstone of our downtown’s rebirth,” Salvatore Testani, president and CEO of Commerce Chenango, said. “Together with the other DRI projects, it stands as a powerful sign of a healthy, growing, and optimistic Norwich.”
The Principle Hotel will have Americans with Disabilities Act (ADA)-compliant features, such as ramps, elevators, and four rooms with accessible bathrooms.
In addition to $3.3 million from the DRI, this project has received $2 million in funding from Empire State Development’s Restore New York initiative, which encourages community development and neighborhood growth through the elimination and redevelopment of blighted structures. The project was also funded through private investments.
“Norwich is building on its strengths and setting the stage for long-term success through its DRI projects, like this boutique hotel, which will allow people to stay overnight right in downtown Norwich,” New York Secretary of State Walter Mosley said. “Here in Norwich, this investment will breathe new life into downtown, by drawing visitors, sparking new business activity and creating lasting opportunities for residents and local entrepreneurs alike.”
Besides the hotel, other DRI projects in Norwich include rehabilitating both the Unguentine Building and the Heritage Building, improving two parks, and enhancing the American Avenue streetscape.
The City of Norwich was named the Southern Tier Region Downtown Revitalization Initiative winner for the fifth round in 2021.
“We are very excited about this project and what it means for the revitalization of downtown Norwich,” Norwich Mayor Brian Doliver said in the state’s announcement about the hotel. “This is an important first step in bringing new life to our city center and can serve as a cornerstone for future economic vitality.”

Visions FCU, SU launch financial-literacy program
SYRACUSE, N.Y. — Syracuse University (SU) is set to launch the Student-Athlete Financial Empowerment Program in January. It’s an initiative designed to prepare Orange student-athletes for long-term financial success during and beyond their college careers. The program will also be open to all SU students, the university said in its Oct. 20 announcement. SU’s Martin
Get Instant Access to This Article
Become a Central New York Business Journal subscriber and get immediate access to all of our subscriber-only content and much more.
- Critical Central New York business news and analysis updated daily.
- Immediate access to all subscriber-only content on our website.
- Get a year’s worth of the Print Edition of The Central New York Business Journal.
- Special Feature Publications such as the Book of Lists and Revitalize Greater Binghamton, Mohawk Valley, and Syracuse Magazines
Click here to purchase a paywall bypass link for this article.
SYRACUSE, N.Y. — Syracuse University (SU) is set to launch the Student-Athlete Financial Empowerment Program in January.
It’s an initiative designed to prepare Orange student-athletes for long-term financial success during and beyond their college careers. The program will also be open to all SU students, the university said in its Oct. 20 announcement.
SU’s Martin J. Whitman School of Management, Syracuse University Athletics, and Visions Federal Credit Union are all teaming up to launch the program.
The program will provide financial-literacy education to more than 550 Syracuse student-athletes across all 20 varsity sports, as well as any SU student interested in enrolling. The school describes it as “among the first of its kind nationally in the post-NIL [name, image, and likeness] era.”
Students will take a for-credit course offered by Whitman School faculty. Through the course’s workshops, one-on-one guidance, and hands-on experiences, students will learn essential skills including budgeting, credit and debt management, investing, wealth protection, and career and post-college financial planning. Student-athletes will be able to leverage what they learn in the program to help them navigate NIL opportunities and tax implications, SU said.
“This partnership reflects our deep commitment to preparing student-athletes not only for success in competition, but also for success in life,” John Wildhack, director of athletics at Syracuse University, said in the school’s announcement. “By combining the Whitman School’s academic expertise with Visions Federal Credit Union’s industry knowledge, we’re equipping our student-athletes with the tools to make smart, confident financial decisions.”
Visions Federal Credit Union will serve as the exclusive financial education partner for the program. Its involvement ensures “consistent, personalized” support for all students, including student-athletes, while also aligning with the credit union’s mission to empower communities through financial wellness.
“At Visions, we believe financial empowerment is life empowerment,” Ty Muse, president and CEO of Visions Federal Credit Union, said. “Partnering with Syracuse Athletics and the Whitman School allows us to invest in the next generation of leaders, helping them build strong financial foundations that will serve them well beyond their playing days.”
The Martin J. Whitman School of Management will play a key role in the program’s academic integration, providing a for-credit academic experience to ensure students are able to learn the tools needed for “financial empowerment offered by Whitman’s nationally ranked expertise in finance and business education.”
“This collaboration exemplifies the best of what Syracuse University offers — an intersection of academics, practical and relevant experience, and community partnership,” Alex McKelvie, interim dean of the Whitman School, said. “We are proud to help our student-athletes develop the skills needed to thrive in a complex business world.”
The Student-Athlete Financial Empowerment Program is part of SU’s Champion ‘Cuse campaign, which is “dedicated to providing student-athletes with the resources, support, and opportunities they need to compete — and succeed — at the highest levels,” the school said.

Beginnings Credit Union formally opens North Syracuse branch
NORTH SYRACUSE, N.Y. — The Beginnings Credit Union branch in the village of North Syracuse has transitioned to its new branding. Formerly CFCU Community Credit Union, Beginnings Credit Union on Oct. 21 held a ribbon cutting at the North Syracuse branch, marking the completion of the building’s update. Beginnings Credit Union says it is updating
Get Instant Access to This Article
Become a Central New York Business Journal subscriber and get immediate access to all of our subscriber-only content and much more.
- Critical Central New York business news and analysis updated daily.
- Immediate access to all subscriber-only content on our website.
- Get a year’s worth of the Print Edition of The Central New York Business Journal.
- Special Feature Publications such as the Book of Lists and Revitalize Greater Binghamton, Mohawk Valley, and Syracuse Magazines
Click here to purchase a paywall bypass link for this article.
NORTH SYRACUSE, N.Y. — The Beginnings Credit Union branch in the village of North Syracuse has transitioned to its new branding.
Formerly CFCU Community Credit Union, Beginnings Credit Union on Oct. 21 held a ribbon cutting at the North Syracuse branch, marking the completion of the building’s update.
Beginnings Credit Union says it is updating all of its branches throughout 2025.
The branch — located at 651 Centerville Place in North Syracuse —had been undergoing updates since the credit union first announced the anticipated rebrand from CFCU to Beginnings in April. The official name change occurred on July 1.
Held in partnership with the Cicero-Plank Road Chamber of Commerce and CenterState CEO, , Beginnings Credit Union members were invited to the event to observe the branch’s updated interior and exterior signage.
“This was a wonderful way to personally introduce the Beginnings brand to our North Syracuse members and the Syracuse community,” Katie Foley, VP of marketing and sales at Beginnings Credit Union, said in the announcement.
Event speakers included Lisa Whitaker, president & CEO of Beginnings Credit Union; Gary Butterfield, mayor of the Village of North Syracuse; and Town of Cicero Supervisor Michael Aregano.
“I have been part of a credit union rebrand in the past, and I can honestly say that the level of energy and excitement from members and staff about the Beginnings rebrand is unmatched,” Michael D’Angelo, VP of member experience at Beginnings Credit Union, contended.
Ribbon-cutting attendees enjoyed refreshments and merchandise giveaways, and Beginnings presented Credit Unions for Kids, benefitting Children’s Miracle Network Hospitals, with donations raised from bottle and can drives at Beginnings’ Waterloo and Cortland Shred Days.
Founded in 1953, Beginnings Credit Union serves nearly 77,000 members. It has $1.4 billion in assets and 15 branch offices. That includes eight offices in Tompkins County, according to its website.

AmeriCU, Mountain Valley FCU merger expected to get state approval by year’s end
ROME, N.Y. — The New York State Department of Financial Services is expected to issue a final approval of the proposed merger between credit unions in the Mohawk Valley and the North Country by the end of the year. The members of Mountain Valley Federal Credit Union in the northeastern part of New York have
Get Instant Access to This Article
Become a Central New York Business Journal subscriber and get immediate access to all of our subscriber-only content and much more.
- Critical Central New York business news and analysis updated daily.
- Immediate access to all subscriber-only content on our website.
- Get a year’s worth of the Print Edition of The Central New York Business Journal.
- Special Feature Publications such as the Book of Lists and Revitalize Greater Binghamton, Mohawk Valley, and Syracuse Magazines
Click here to purchase a paywall bypass link for this article.
ROME, N.Y. — The New York State Department of Financial Services is expected to issue a final approval of the proposed merger between credit unions in the Mohawk Valley and the North Country by the end of the year.
The members of Mountain Valley Federal Credit Union in the northeastern part of New York have voted to merge their credit union with AmeriCU Credit Union, which is headquartered in Rome.
Mountain Valley Federal Credit Union is based in Peru in Clinton County, south of Plattsburgh. Mountain Valley members voted by mail and in-person at a special membership meeting on Sept. 18.
The proposed merger will enable the nonprofit Upstate New York credit unions to expand access to services, expertise, and branch locations for members and businesses across the Northern and Central New York regions, per AmeriCU’s Sept. 22 announcement.
The merger has also been approved by the National Credit Union Administration (NCUA), the federal agency that regulates federal credit unions.
AmeriCU has been serving members who live or work in Clinton and Essex counties for a number of years. The expanded AmeriCU credit union will serve more than 180,000 members across 24 counties, with 25 locations and combined assets of $2.8 billion, the Rome–based credit union said.
Mountain Valley’s four branch locations — all in Clinton and Essex counties — will become AmeriCU branches and make up AmeriCU’s Mountain Valley Region. All Mountain Valley employees have been offered the chance to continue working for the combined organization.
Ron Belle, president and CEO of AmeriCU Credit Union, will continue in that role in the combined organization. Mountain Valley CEO Maggie Pope will become assistant VP for community engagement in AmeriCU’s newly developed Mountain Valley Region. Pope is a well-known and highly regarded business leader in Clinton and Essex Counties, AmeriCU noted in its announcement.
Mountain Valley FCU initiated the merger and its board of directors unanimously approved it earlier this year, “citing the many similarities in the organizations’ origins, foundational values, commitment to member satisfaction, and community involvement.”
“My dad would be so proud,” said Kathleen Roach, president of Mountain Valley board of directors, whose late father, John Roach, founded the credit union in 1963.
John Roach was a teacher in the Peru Central School District, per the AmeriCU announcement.

AmeriCU appoints senior VP of marketing
ROME, N.Y. — AmeriCU Credit Union recently announced it has hired Amber Cooleen as its new senior VP of marketing. She recently spent four years serving as chief marketing officer for a credit union based in the Capital Region. Throughout her career, Cooleen has held key marketing roles across various industries, from business-to-business startups to
Get Instant Access to This Article
Become a Central New York Business Journal subscriber and get immediate access to all of our subscriber-only content and much more.
- Critical Central New York business news and analysis updated daily.
- Immediate access to all subscriber-only content on our website.
- Get a year’s worth of the Print Edition of The Central New York Business Journal.
- Special Feature Publications such as the Book of Lists and Revitalize Greater Binghamton, Mohawk Valley, and Syracuse Magazines
Click here to purchase a paywall bypass link for this article.
ROME, N.Y. — AmeriCU Credit Union recently announced it has hired Amber Cooleen as its new senior VP of marketing.
She recently spent four years serving as chief marketing officer for a credit union based in the Capital Region. Throughout her career, Cooleen has held key marketing roles across various industries, from business-to-business startups to global real-estate organizations.
With more than 20 years of experience, Cooleen “brings innovation, creativity, and a proven record of leadership to help support AmeriCU’s growth,” the credit union contended in its Aug. 25 announcement.
Cooleen indicated that her focus will be on strengthening the credit union’s connection with its members, reinforcing that members can count on AmeriCU.
“Our members are at the center of everything we do, and it’s critical that we connect with them in a meaningful, impactful manner,” Cooleen said in the announcement. “Our members have many choices for where they open a checking account, get a car loan, or apply for a mortgage. What sets us apart is the relationships we have with them — we aren’t just a credit union, we are a trusted financial partner.”
Cooleen holds a bachelor’s degree in English with a concentration in writing, along with a master’s degree in corporate and organizational communications from Fairleigh Dickinson University in New Jersey.
Beyond her professional accomplishments, Cooleen has volunteered with organizations such as Catherine’s Center for Children and the Red Cross of Northeastern NY, where she served three years on the board of directors. She has also volunteered as a judge for the America’s Credit Unions’ Diamond Awards, an annual credit union marketing competition.
The nonprofit AmeriCU Credit Union is a member-owned, financial institution with total assets of $2.8 billion and more than 170,000 members in New York state and beyond.

New Visions FCU chief HR officer wants to listen and learn
ENDWELL, N.Y. — Visions Federal Credit Union (FCU) has a new VP/chief human resources officer (CHRO), who started her new duties back in the summer. For Aoife Quinn, the priority early on has been to listen and learn. “After getting a sense of who we are, where we are, and where we want to be,
Get Instant Access to This Article
Become a Central New York Business Journal subscriber and get immediate access to all of our subscriber-only content and much more.
- Critical Central New York business news and analysis updated daily.
- Immediate access to all subscriber-only content on our website.
- Get a year’s worth of the Print Edition of The Central New York Business Journal.
- Special Feature Publications such as the Book of Lists and Revitalize Greater Binghamton, Mohawk Valley, and Syracuse Magazines
Click here to purchase a paywall bypass link for this article.
ENDWELL, N.Y. — Visions Federal Credit Union (FCU) has a new VP/chief human resources officer (CHRO), who started her new duties back in the summer.
For Aoife Quinn, the priority early on has been to listen and learn.
“After getting a sense of who we are, where we are, and where we want to be, my focus will be translating those insights into clear priorities that strengthen our culture, deepen employee engagement, and reinforce the trust our employees and members place in us,” Quinn said. “We’re building alignment and momentum for the future — ensuring that our people strategy is a lever for growth, impact, and long-term value.”
Quinn comes to Visions FCU with 30 years of experience in human resources (HR), per the Sept. 9 announcement. She also has experience in change management, workplace culture transformation, and executive leadership coaching with corporate clients, and global, multicultural SaaS (software as a service) enterprises for more than a decade.
Prior to joining Visions FCU, Quinn worked as VP/people & culture, head of global human resources at Utopus Insights, which is based in Valhalla in Westchester County. In that role, she led all HR activity for the renewable-energy analytics organization across 10 countries.
In three years, Quinn implemented HR strategies that drove engagement and recruitment, reduced turnover, and supported a positive workplace culture. During that time, she also provided her leadership in change management as Utopus Insights was acquired by and integrated into Vestas Wind Technologies, Visions FCU said.
“I’ve consistently been drawn to organizations, like Visions, that prioritize the employee experience,” Quinn said. “I’m driven by the opportunity to shape an inclusive workplace culture where everyone has a chance to thrive.”
Visions FCU’s workforce includes more than 900 full-time employees across its three-state footprint in New York, New Jersey, and Pennsylvania. In addition to providing financial services, the credit union emphasizes “people helping people” and includes service and community as two of its corporate values, the credit union noted.
Visions FCU went on to say that Quinn has already noticed how these values “resonate among the workforce.”
“I’ve already met so many individuals who are not only deeply passionate about their work but also kind, intellectually curious, and engaged in the world beyond their day-to-day roles,” she said.
Established in 1966, the nonprofit Visions Federal Credit Union serves more than 250,000 members in communities throughout New York, New Jersey, and Pennsylvania. Services include banking as well as auto, home, personal, and business loans.

CNY banking leader sees solid area business conditions, outlook
Region is buoyed by Micron project SYRACUSE, N.Y. — Even as stock markets continue to make all-time highs, there has been a lot of chatter about national economic uncertainty this year with slowing job growth and concern about the potential impact of tariffs, continued inflation, and most recently the federal-government shutdown. But current conditions and
Get Instant Access to This Article
Become a Central New York Business Journal subscriber and get immediate access to all of our subscriber-only content and much more.
- Critical Central New York business news and analysis updated daily.
- Immediate access to all subscriber-only content on our website.
- Get a year’s worth of the Print Edition of The Central New York Business Journal.
- Special Feature Publications such as the Book of Lists and Revitalize Greater Binghamton, Mohawk Valley, and Syracuse Magazines
Click here to purchase a paywall bypass link for this article.
Region is buoyed by Micron project
SYRACUSE, N.Y. — Even as stock markets continue to make all-time highs, there has been a lot of chatter about national economic uncertainty this year with slowing job growth and concern about the potential impact of tariffs, continued inflation, and most recently the federal-government shutdown.
But current conditions and the outlook for the Central New York economy and business climate are not really showing those problems, says one local banking expert.
“I’ll be honest there hasn’t been much shift. We’re not really seeing much negativity,” says Lindsay Weichert, Community Bank, N.A.’s regional president for the Central New York market. “Margins are really holding up. Revenues and sales are holding up well, pretty much across our book of clients.”
Weichert spoke with CNYBJ on Oct. 16. In her position, she is responsible for leading Community Bank’s business development and community-engagement activities while ensuring effective communication across all bank and non-bank lines of business in the Central New York region.
Weichert says tariffs have not yet created many impacts for her bank’s clients, inflation has steadied some, and interest rates have ticked down in recent months.
“We’re still seeing kind of just the normal business cycle. It’s end of year; folks are evaluating equipment purchases. [Clients] still seem kind of unphased by the economy. So we’re not really seeing any pullbacks, anything like that,” she says.
One indicator Weichert looks at to gauge how businesses are doing, is their credit-line usage.
“You expect that if there is broad concern with the economy, they may borrow, throw some cash into an account, and sort of sit tight,” she explains. The bank is not seeing that. Credit-line usage is “totally within a normal range. It’s actually down a little bit from a couple months back,” Weichert notes.
The Micron effect
“It’s really kind of business as usual. And I think we do have a pretty significant advantage here in Syracuse relative to some of the rest of the country with Micron,” Weichert says, referring to Micron Technology’s (NASDAQ: MU) project to build a massive semiconductor campus at the White Pines Commerce Park in the town of Clay. “That provides some pretty good certainty… it’s pretty nice to know that by the end of next year we’ll have 5,000 construction workers on site.”
Even before that, the stage is being set within the community.
“We’re really starting to build out a talent pipeline …you can see it in the higher education space between OCC, Syracuse University, CenterState CEO, all these different folks, MACNY, kind of gearing up to really focus on the apprenticeship program and build on the talent pipeline,” says Weichert. “That sort of feeds on itself and attracts more folks into our market. And then just the multiplier effect. You get 5,000 people as an influx into the community, there is no way they’re not spending a couple bucks while they’re here.”
Micron says it expects to create 9,000 jobs directly over the next 20 years or so.
“But then that multiplier effect is like 5 or 6 [times that] for all the ancillary businesses. So, all those folks are renting and purchasing homes. And going out and patronizing the restaurants, and so on and so forth,” says Weichert.
That helps provide a foundation that there is going to be a certain amount of economic growth going forward in our area and helps allay some concerns about the variability of the broader national and global economy.
Get our email updates
Stay up-to-date on the companies, people and issues that impact businesses in Syracuse, Central New York and beyond.
